Performance Management in Healthcare: Challenges & Best Practices
.svg)

.svg)

Effective performance management in this healthcare aligns individual clinical actions with broader hospital goals, such as reducing readmission rates, improving patient satisfaction, and maintaining strict compliance with health regulations.
In this article, we’ll examine how healthcare organizations can transition from burdensome, paper-based annual reviews toward continuous, data-driven feedback to address staff burnout and ensure clinical excellence.
Healthcare is defined by thin margins and high stakes, so the way you manage people directly dictates the quality of care provided. Establishing a structured performance system ensures that every staff member understands their role in the patient's journey.
Staff with clearly defined clinical goals are significantly more efficient. Clear expectations reduce time spent on administrative ambiguity, allowing more time for direct patient interaction.
Healthcare organizations with strategic performance approaches are twice as likely to retain specialized staff, mitigating the high costs of nursing turnover and burnout that go beyond financial consequences and can extend to patient care.
Documented performance objectives establish a fair foundation for credentialing, protecting against bias and ensuring that clinical standards are met across all shifts.
Connecting individual targets to hospital-wide initiatives, like reducing hospital-acquired infections, ensures the entire facility moves in the same direction.
Systematic reviews identify skill gaps early, allowing for targeted training in new medical technologies or specialized patient care techniques.
Healthcare is a dynamic environment, so rapid changes in this industry are to be expected, but many legacy evaluation systems are struggling to keep pace. Identifying these friction points is the first step toward building a more resilient workforce.
With the rise of remote diagnostics, managers struggle to provide timely feedback to distributed teams who aren't physically present on the hospital floor.
Waiting for annual reviews is dangerous in medicine. Delayed course corrections can lead to clinical errors or prolonged inefficiencies.
Manual tracking consumes a significant amount of a manager’s time. This "paperwork tax" pulls clinical leaders away from mentoring their staff.
Without a clear cascade of priorities, staff may hit individual task targets while the department misses larger strategic objectives like patient satisfaction scores.
When systems feel opaque or subjective, clinicians disengage. Fairness is essential for maintaining morale in high-pressure environments.
Adopting modern performance standards allows clinical leaders to move from "policing" behavior to coaching for excellence. These practices ensure that evaluations support the high-stakes environment of patient care.
Shift away from the high-pressure annual review. Brief bi-weekly or monthly touchpoints allow managers to address patient safety concerns, caseload management, and immediate obstacles in real-time.
Use 90-day targets rather than annual goals. This agility is necessary to keep pace with shifting hospital protocols, new medical technologies, and seasonal patient volume fluctuations.
Performance tracking should live where the work happens, such as within Microsoft Teams. Reducing the "software switch" prevents administrative burnout and ensures clinical data is recorded accurately.
Create a "safe space" for staff to discuss skill gaps or "near-miss" clinical errors. When growth conversations are separated from salary discussions, clinicians are more honest about where they need support.
Success in healthcare relies heavily on effective communication. Gathering input from nurses, physicians, and technicians provides a holistic view of a staff member’s collaborative impact and professional conduct on the floor.
To drive quality improvement, healthcare organizations must move beyond generic metrics. These Key Performance Indicators (KPIs) provide a data-driven lens through which to view both staff engagement and clinical efficacy.
A clinical performance review should prioritize patient safety, technical competence, and collaborative care. This structured approach provides clarity on medical standards while leaving room for meaningful dialogue about professional growth.
Role: Clinical Nurse Manager
Core Skill Areas:
Performance Review Questions:
Performance Rating Criteria:
Development Plan Components:
Even with the best intentions, outdated management habits can create a culture of "compliance over care." Recognizing these errors is the first step toward a more empowered medical staff.
Managers who don't keep written records fall victim to recency bias. A single mistake in December shouldn't outweigh eleven months of exceptional patient care.
Using the same KPIs for a trauma surgeon and a receptionist is ineffective. Metrics must reflect the specific technical competencies and patient-facing responsibilities of each role.
Telehealth providers and night-shift staff often suffer from lower visibility. Performance systems must ensure these remote or off-cycle workers receive equal access to recognition and promotion.
If the ICU grades more strictly than the Pediatrics department, internal mobility and fairness suffer. Regular calibration sessions ensure a "meets expectations" rating is uniform across the facility.
When performance management feels like a bureaucratic requirement rather than a tool for clinical growth, staff disengage. The process must yield actionable insights that improve the daily work of the clinician.
Performance management in healthcare is evolving toward data-driven, AI-enhanced, and patient-centered models to address staffing shortages, rising costs, and quality demands. Key trends emphasize continuous feedback, technology integration, and resilience-focused metrics tailored to the industry's unique challenges.
The table below summarizes these key trends:
FHIR APIs enable seamless, real-time interoperability across EHRs, wearables, and apps, supporting performance metrics tied to population health and clinician efficiency. This standard reduces data silos, cutting administrative burdens in exchanges and improving outcome tracking for value-based care, as seen in Google Cloud's FHIR implementations.
Studies on Flat FHIR exports show it scales for bulk data access, aiding cohort analysis without custom ETL, which enhances PM by linking clinical decisions to shared metrics
Focus on value-based care ties performance to patient outcomes over volume, with risk-sharing and bundled payments incentivizing quality. One aspect of this trend is payer-provider collaborations using AI for prior authorizations, cutting manual efforts via real-time data networks. Moreover, a study also found high-quality metrics in PM enhance trust and performance in healthcare settings.
AI and machine learning are transforming performance evaluation by enabling predictive staffing, burnout detection, and personalized development plans. For instance, AI stewardship tools flag low-value interventions, potentially reducing inpatient costs without quality loss.
Shifts from annual reviews to real-time, agile feedback via OKR software like Teamflect improve accountability and employee well-being. AI-powered modules can detect burnout early, integrating wellness KPIs to sustain productivity. Research on HTA-PM integration also stresses evidence-based metrics aligning tech adoption with outcomes, boosting hospital resilience.
Teamflect integrates directly into Microsoft Teams to streamline clinical and administrative workflows. Large-scale healthcare organizations require tools that balance rigorous compliance with extreme ease of use for frontline staff. The following examples highlight how medical imaging and long-term care leaders transitioned from fragmented, manual methods to unified, automated systems through Teamflect.
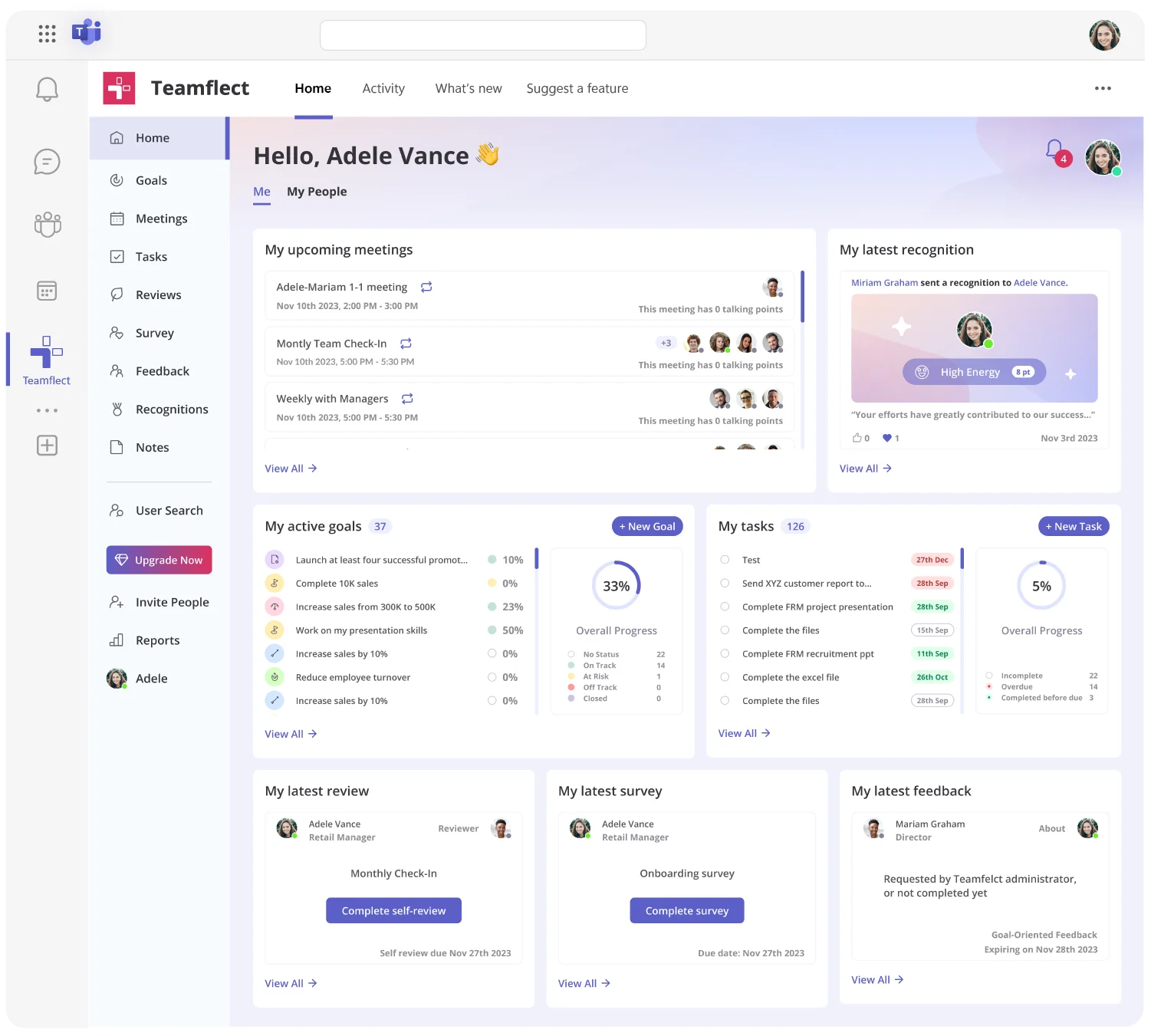
Healthcare performance management must operate within fast-paced clinical environments where time is limited and accuracy is critical. Teamflect's performance management software enables healthcare leaders to support clinical staff development without interrupting patient care workflows.
MedQuest, a medical imaging management company with over 1,000 frontline employees, transitioned from informal reviews to a sophisticated pay-for-performance culture.
Invacare, a global manufacturer of home and long-term care medical products, used Teamflect to unify fragmented HR processes across 22 countries.
Performance management looks different across industries based on unique sector requirements. This snapshot shows key distinctions.
Each industry requires tailored approaches, but all benefit from clear expectations, regular feedback, and systems that reduce administrative burden while improving evaluation quality.
Shift from subjective opinions to objective data. Use 360-degree feedback from nurses, physicians, and administrative peers to capture a full picture of clinical conduct. Documenting performance throughout the year prevents bias and ensures the review reflects a consistent standard of care across different shifts and departments.
Keep brief, dated notes on one-on-one check-ins, specifically noting progress on clinical certifications or patient care goals. Record specific instances of excellence or safety concerns as they happen to provide clear context during credentialing or annual evaluations.
Conduct calibration sessions at least quarterly. Because patient care standards must be uniform, managers from different units should review ratings together to ensure a "meets expectations" grade in Radiology carries the same weight and rigor as one in Intensive Care.
Address gaps immediately to protect patient safety. Distinguish between skill gaps, resource shortages, or burnout. Create a focused improvement plan with measurable clinical milestones and provide support through mentorship or additional training before moving to formal disciplinary steps.
The primary hurdle is time poverty. Clinicians often spend hundreds of hours on paperwork. Other challenges include recency bias, where a single recent medical error might overshadow months of excellent care, and the difficulty of maintaining visibility over staff working rotating night or weekend shifts.
An all-in-one performance management tool for Microsoft Teams
